That sudden, intense, "gotta go right now" feeling—it's more than just an inconvenience. If you find yourself constantly rushing to the restroom, or if those intense urges sometimes lead to leaks, you're experiencing symptoms of Overactive Bladder (OAB). Put simply, OAB is a common, manageable medical condition where the bladder muscle contracts involuntarily, even when the bladder isn't full. It can severely impact your daily routine, sleep, and overall quality of life, making you constantly plan your day around bathroom access. But here's the good news: you are not alone, and there are effective treatments and strategies to regain control.
What is an overactive bladder (OAB)?
According to the International Continence Society (ICS), Overactive Bladder (OAB) is defined by the presence of urinary urgency, usually accompanied by frequency (urinating too often) and nocturia (waking up to urinate at night), with or without urgency urinary incontinence.
💡 Essentially, OAB is a symptom complex, not a disease, characterized by the sudden, difficult-to-defer desire to urinate.
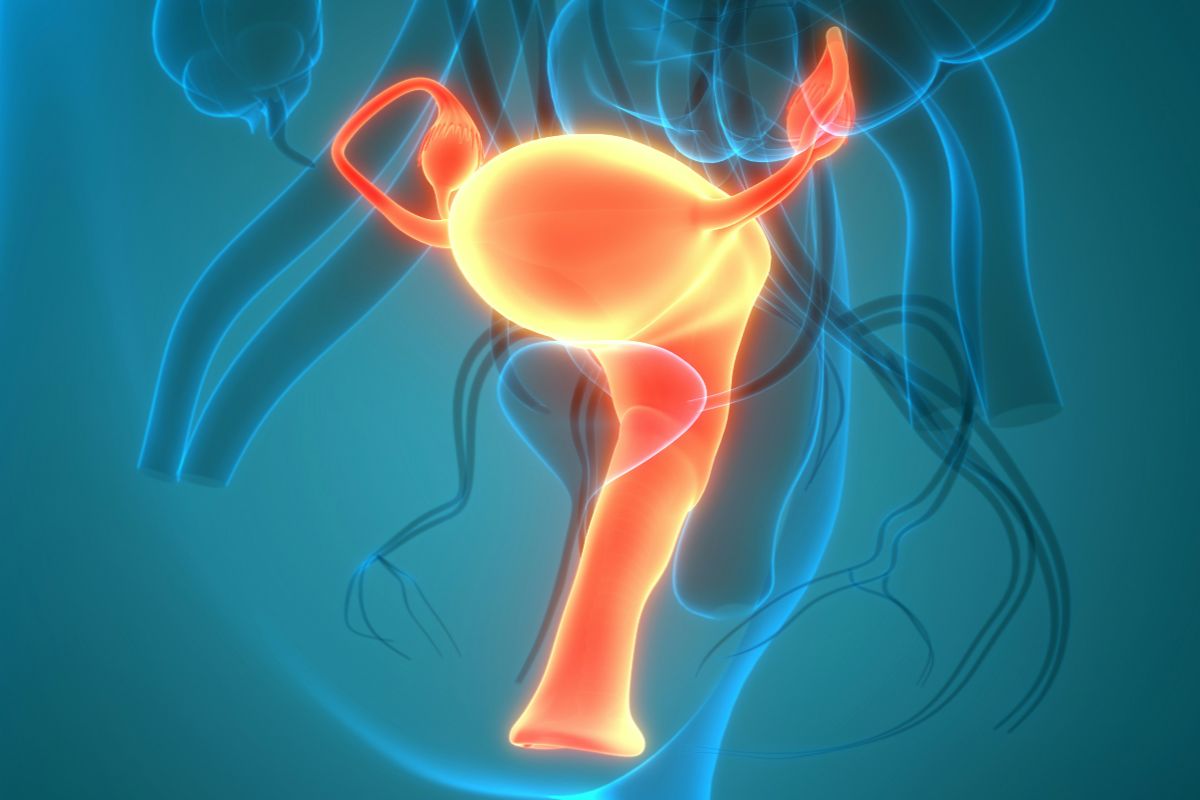
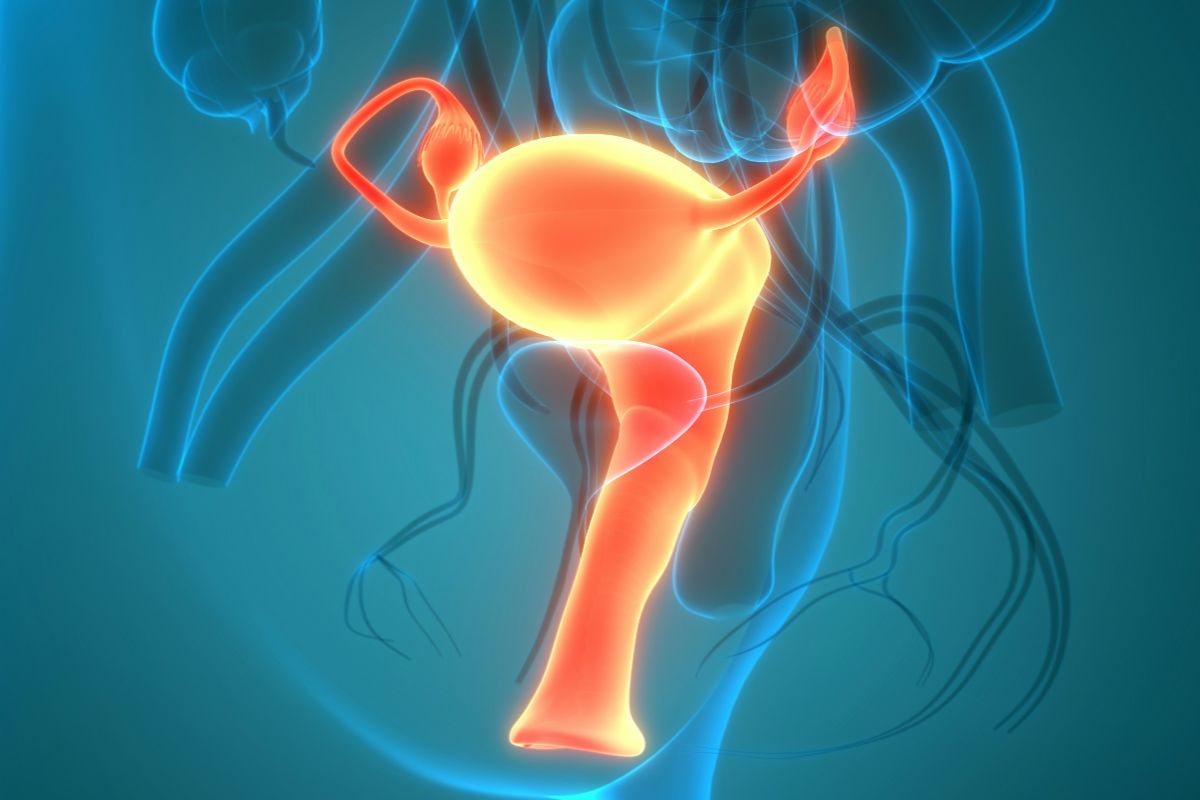
This feeling is caused by an involuntary contraction of the detrusor muscle in the bladder wall,often reflecting disrupted communication between the bladder, pelvic floor muscles, and nervous system rather than a structural abnormality alone.
It's important to know there are two types of OAB:
- "Wet" OAB: This occurs when the urgency is accompanied by accidental urine leakage (urinary incontinence).
- "Dry" OAB: This is OAB without any leakage or incontinence.
OAB is remarkably common, affecting millions of Americans and significantly increasing with age. It's not a normal part of aging, but a treatable condition. Recognizing these symptoms is the first step toward getting help and regaining control over your life.
Common overactive bladder symptoms to watch for
The symptoms of OAB are more than just a nuisance; they are the signs that your bladder's signaling system is overly sensitive. Understanding these core symptoms helps you accurately describe your condition to a healthcare provider.
- Urinary urgency: This is the hallmark symptom and the most disruptive. It’s a sudden, compelling desire to pass urine which is difficult to postpone. This intense feeling often dictates your activities and causes significant anxiety.
- Urinary frequency: Defined as urinating more than eight times in a 24-hour period. This constant need to void means you are frequently seeking out restrooms, whether at work, during errands, or while traveling. It's a significant drain on your productivity and freedom.
- Nocturia: This is the need to wake up one or more times during the night specifically to urinate. Nocturia severely fragments sleep, leading to chronic fatigue, poor concentration, and a lower quality of life. Consistent sleep interruption due to bladder urges can also impact overall health and mood.
💡 These symptoms often create a cycle of fear and preemptive bathroom trips, where you void "just in case", which unintentionally trains the bladder to tolerate smaller volumes and reinforces urgency patterns over time.
Addressing these behaviors is a key part of effective OAB management.
What causes an overactive bladder?
The exact cause of Overactive Bladder (OAB) isn't always clear, but it often involves a combination of factors that disrupt the normal communication between the bladder, nerves, and brain. These factors lead to the involuntary and untimely contractions of the detrusor muscle. Understanding potential triggers is crucial for successful treatment and management:
- Abnormal bladder muscle contractions (detrusor instability): The detrusor muscle, which lines the bladder, may contract too early, signaling an urge to urinate before the bladder is actually full.
- Nerve damage: Conditions that affect the nervous system, such as Multiple Sclerosis (MS), Parkinson’s disease, stroke, or injury to the spinal cord, can interfere with the nerve signals that tell the brain when the bladder is full.
- Excess fluid intake or irritants: Drinking large amounts of fluid, especially caffeine, alcohol, or acidic beverages, can irritate the bladder lining and increase both the volume of urine and the frequency of urges.
- Aging: While not a normal part of aging, changes in bladder capacity, muscle strength, and hormone levels as we age can contribute to OAB symptoms.
- Underlying medical conditions: Conditions like poorly controlled diabetes, Urinary Tract Infections (UTIs), bladder stones, or bladder tumors can mimic or exacerbate OAB symptoms.
- Bladder outlet obstruction: In men, an enlarged prostate (Benign Prostatic Hyperplasia - BPH) can obstruct flow, leading to incomplete emptying and an overstressed, overactive bladder.
Identifying and addressing these underlying factors is a primary goal in managing your OAB symptoms. Pelvic floor muscle dysfunction—whether weakness, poor coordination, or delayed activation—can also contribute by reducing the body’s ability to inhibit involuntary bladder contractions.
Diagnosing overactive bladder: what to expect
Getting an accurate diagnosis is the essential first step toward finding relief. Since OAB symptoms can overlap with other conditions, your healthcare provider (Urologist, Urogynecologist, or Physical Therapist) will follow a thorough process to rule out other causes.
- Initial consultation and medical history: The process starts with a detailed discussion of your symptoms, their duration, frequency, severity, and how they impact your quality of life. They will review your general health, medications, and fluid intake habits.
- Physical examination: A physical exam will be performed, which may include a neurological assessment and a pelvic exam (for women) or a digital rectal exam (for men) to check muscle tone and rule out underlying issues.
- Voiding/bladder diary: This is often the most important diagnostic tool. You will be asked to track the time and volume of every void, along with fluid intake and episodes of urgency or leakage, typically over three to seven days. This objective data helps define the severity of your OAB and guides treatment.
- Urine analysis (Urinalysis): A urine sample will be tested to check for signs of infection (UTI), blood, or glucose (which may indicate undiagnosed diabetes), as these conditions can mimic OAB symptoms.
- Post-void residual (PVR) measurement: This test uses a simple ultrasound to see how much urine is left in your bladder after you try to empty it. Significant residual urine can contribute to frequency.
- Advanced tests (Urodynamics): If initial treatments fail or the diagnosis is unclear, specialized testing (like urodynamic studies) may be ordered to measure bladder pressures, volumes, and function during filling and emptying.
This systematic approach ensures that your treatment plan specifically targets your overactive bladder symptoms, rather than a different underlying issue.
Lifestyle and behavioral changes for overactive bladder
The most accessible and often most effective first-line treatment for OAB involves making strategic changes to your daily habits. These non-invasive steps empower you to manage your symptoms and take back control of your bladder.
1. Bladder retraining (scheduled voiding)
Bladder retraining is a technique designed to gradually increase the time between bathroom trips, effectively resetting the bladder-brain connection. The goal is to suppress the urge rather than immediately giving in.
- How to start: Keep a detailed bladder diary for several days to determine your current average interval between voids.
- The schedule: Start by setting a fixed voiding schedule based on this interval (e.g., every 60-90 minutes), whether you feel the urge or not.
- Suppress the urge: When the sudden urge strikes before your scheduled time, use distraction, deep breathing, or a quick squeeze and lift of the pelvic floor muscles (a "quick flick" Kegel) to suppress the urge until the scheduled time.
- Gradual increase: Gradually lengthen the interval between scheduled voids by 15-30 minutes every week or two. Over time, this helps your bladder hold more urine and reduces the feelings of urgency and frequency.
2. Dietary modifications
What you drink and eat can significantly irritate the bladder lining, triggering spasms and urgency.There is no single “overactive bladder diet”, but identifying and reducing individual bladder irritants is a key component of symptom control. Modifying your intake is a simple yet powerful tool.
- Reduce bladder irritants: The most common culprits are caffeine (found in coffee, tea, and soda), alcohol, carbonated beverages, and highly acidic foods (like citrus fruits, tomatoes, and spicy foods). Try eliminating one irritant at a time for two weeks to see if symptoms improve.
- Manage fluid intake: While you shouldn't drastically restrict fluids (which can lead to dehydration or concentrated, irritating urine), manage when you drink. Adequate daytime hydration with gradual evening fluid reduction supports bladder health and helps minimize nocturia (waking up at night to void) without increasing irritation from concentrated urine.
- Fight constipation: A full bowel places pressure on the bladder, worsening OAB symptoms. Ensure adequate intake of fiber and water to maintain regular bowel movements.
3. Pelvic floor muscle training (Kegels)
Often referred to as Kegel exercises, strengthening the pelvic floor muscles is crucial for managing urgency and preventing urgency-related leakage.
- The mechanism: The pelvic floor muscles wrap around the urethra. A strong, quick contraction (the "quick flick") acts as a temporary sphincter closure and sends a signal to the brain that overrides the urgency signal,activating the detrusor inhibitor reflex and helping the detrusor muscle relax.
- How to perform: Contract the muscles as if you are trying to stop the flow of urine and prevent passing gas simultaneously. Focus on a strong, quick lift, not just a squeeze.
- Integration: The key is to use the muscles reactively—perform a quick, strong contraction immediately when you feel the first sign of urinary urgency or when having a bladder leak. This technique is called the Knack. Regular, consistent training (holding contractions for 5-10 seconds, repeated 10 times, 3 times a day) builds the endurance needed for support.
For best results with these exercises, consultation with a Pelvic Floor Physical Therapist is highly recommended to ensure proper technique and tailor a specific program to your needs.
Is Perifit Care or Care+ Can help you with overactive bladder?
The mechanism: training the detrusor inhibitor reflex
The core of the Perifit approach for OAB lies in its Urge Incontinence program. This program focuses specifically on training your levator ani muscles (the main part of the pelvic floor) to trigger a natural protective reflex called the detrusor inhibitor reflex (or Mahony reflex).
💡 When trained correctly, a strong, sustained pelvic floor contraction can automatically suppress the overactivity of the detrusor muscle in your bladder, thereby reducing the sudden, intense urge to urinate.
What the program targets
The device's training emphasizes specific muscle characteristics crucial for OAB relief:
- Endurance: Training with lower strength at longer intervals specifically targets the slow-twitch muscle fibers. This prolonged squeeze helps to sustain the inhibitory reflex, calming the bladder and allowing you to defer the urge.
- Strength: Developing sufficient strength is essential to ensure continence and stop immediate leaks associated with urgency.
What can you expect?
Clinical research supports the benefits of consistent PFMT:
- Clinical research supports pelvic floor muscle training as an effective first-line approach for reducing urgency-related leakage and improving quality of life.
- Women report reduced daily leaks, less time spent planning around bathrooms, and an improved quality of life.
Living with the relentless urgency, frequency, and potential leakage of overactive bladder (OAB) can feel isolating and restrictive, but this journey has shown that it is a highly treatable condition. Remember that the foundational, non-invasive steps—including simple behavioral changes like bladder retraining and strategic dietary modifications—often provide significant relief.
By mastering your pelvic floor muscles through targeted exercises (like Kegels) and adopting urgency suppression techniques, you can actively reduce spasms and regain confidence.
Sources: