
How do you know if Kegels are working?
Curious about your Kegel progress? You're not alone in wondering how long it takes for Kegels to show results and how to tell if those pelvic floor exercises are actually making a difference.

Experiencing pelvic pain after running? Here's why
Ouch! That post-run pelvic pain can really put a damper on your running routine. If you're experiencing discomfort down there after pounding the pavement, you're probably wondering what's going on.

Pelvic floor yoga: strengthen and restore harmony
Is your pelvic floor in need of some extra care and attention? Practicing yoga could be the ideal solution you've been seeking. This ancient practice isn't just about striking poses on a mat - it c...

Pilates for pelvic floor strengthening and support
Pilates offers a wealth of benefits for your pelvic floor muscles, which play a crucial role in supporting your core and maintaining continence.

Pelvic floor and tailbone pain: what it means & how to treat it?
Have you ever experienced an unrelenting aching sensation in your pelvic region or tailbone? Pelvic floor dysfunction and tailbone pain are more common than you might think, affecting people of all...

Pelvic floor orgasm: your key to unforgettable pleasure
Ever wondered about the secret to mind-blowing orgasms? It might be right under your nose—or rather, between your legs. The pelvic floor, often overlooked, plays a crucial role in sexual pleasure. ...
Pelvic floor release exercises: soothe and unwind
Ever felt like your pelvic area is a bundle of knots? You're not alone. Pelvic floor tension is more common than you might think, affecting people of all ages and backgrounds.

Pelvic floor breathing exercises: enhance your wellbeing
Ever wondered about those mysterious pelvic floor breathing exercises everyone's talking about? These powerful yet subtle techniques can work wonders for your overall wellbeing.

Tackling weak pelvic floor in your 20s
Ever noticed those little leaks when you laugh or sneeze? Or maybe you're feeling things aren't quite right down there?

Vulva vs. Vagina: what's the difference & why it matter?
Let us begin a discussion about a topic that is commonly misunderstood yet crucially significant: the difference between vulva and vagina. Yep, they're not the same thing!
Does queefing really mean you have a weak pelvic floor?
Have you ever been in an embarrassing scenario where air escaped from your lower body during an intimate moment or yoga class? Yep, we're talking about vaginal queefs - those unexpected (and someti...

Can vitamins help pelvic floor dysfunction?
Ever felt like your pelvic floor could use a little extra support? It can happen. Pelvic floor dysfunction is more common than you might think, and it can really put a damper on your day-to-day life.

What foods help strengthen pelvic floor muscles?
Ever wondered if your diet could give your pelvic floor a boost? Many people are curious about how what's on their plate might impact their pelvic health.

Manage pelvic floor dysfunction with this food avoidance guide
Living with pelvic floor dysfunction can be a real challenge, especially when it comes to figuring out what to eat. You might feel like you're walking on eggshells with every meal, unsure if your n...

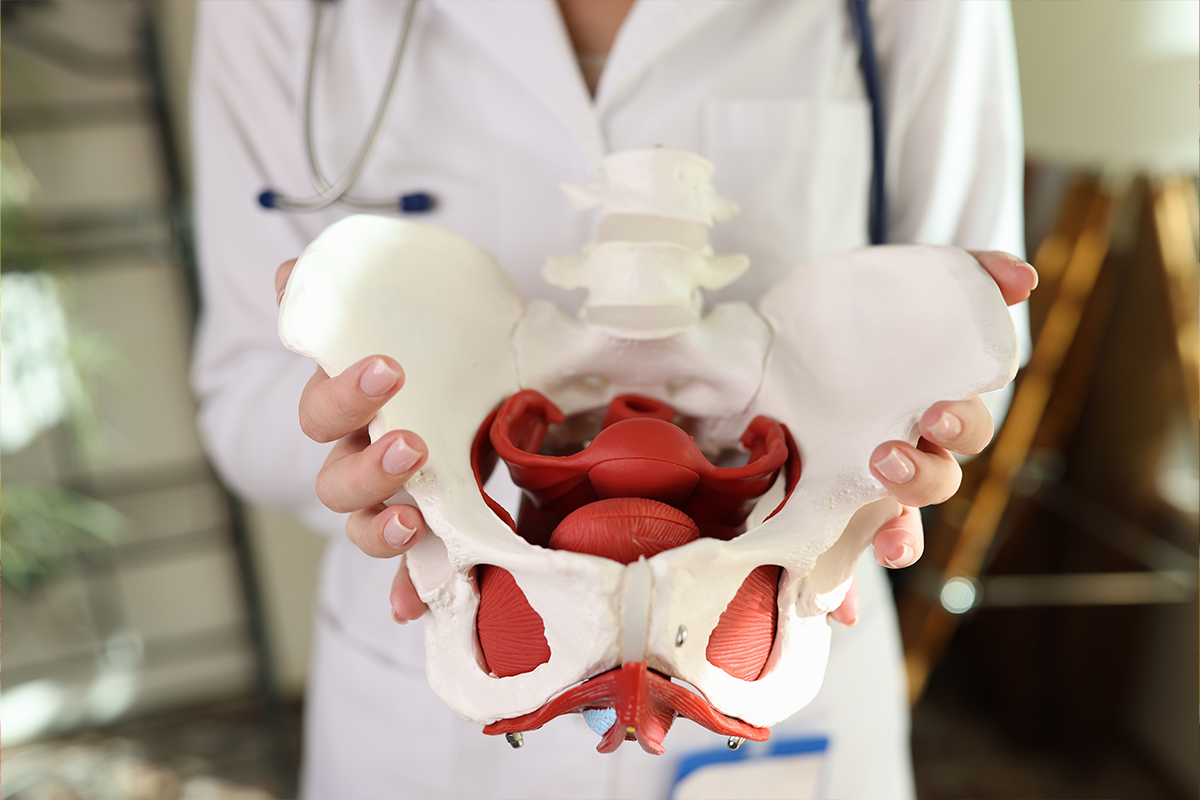
Pelvic floor biofeedback: your key to stronger muscles
Ever felt like your pelvic floor muscles could use a little boost? Pelvic floor biofeedback might just be the secret weapon you've been looking for.

Ever experienced that awkward moment when you cough and suddenly feel a little leak? You're not alone! Peeing when coughing is more common than you might think.

Peeing during sex: what's normal and when to worry?
Ever felt the urge to pee during intercourse? You're not alone! Many people experience bladder sensations or even leakage while getting intimate.

How to tell if your pelvic floor muscles are tight or weak?
Ever feel like your pelvic floor is playing tricks on you? Whether you're dealing with unexpected leaks, pelvic pain, or just feeling a bit "off" down there, your pelvic floor muscles might be the ...

Exercises to avoid with a weak pelvic floor
If you're dealing with a weak pelvic floor, you might be wondering which exercises are safe and which ones to avoid. Don't worry, we've got you covered!

Deep core and pelvic floor exercises for a strong foundation
Whether you're dealing with postpartum recovery, sneaky leaks, or just want to stand taller, it's time to dive into the world of deep core and pelvic floor exercises.

Pelvic floor pain after exercising: why is this happening?
Ever finished a workout feeling great, only to be hit with unexpected pelvic pain later? You are not the only one in this situation. Many people experience discomfort down there after exercising.
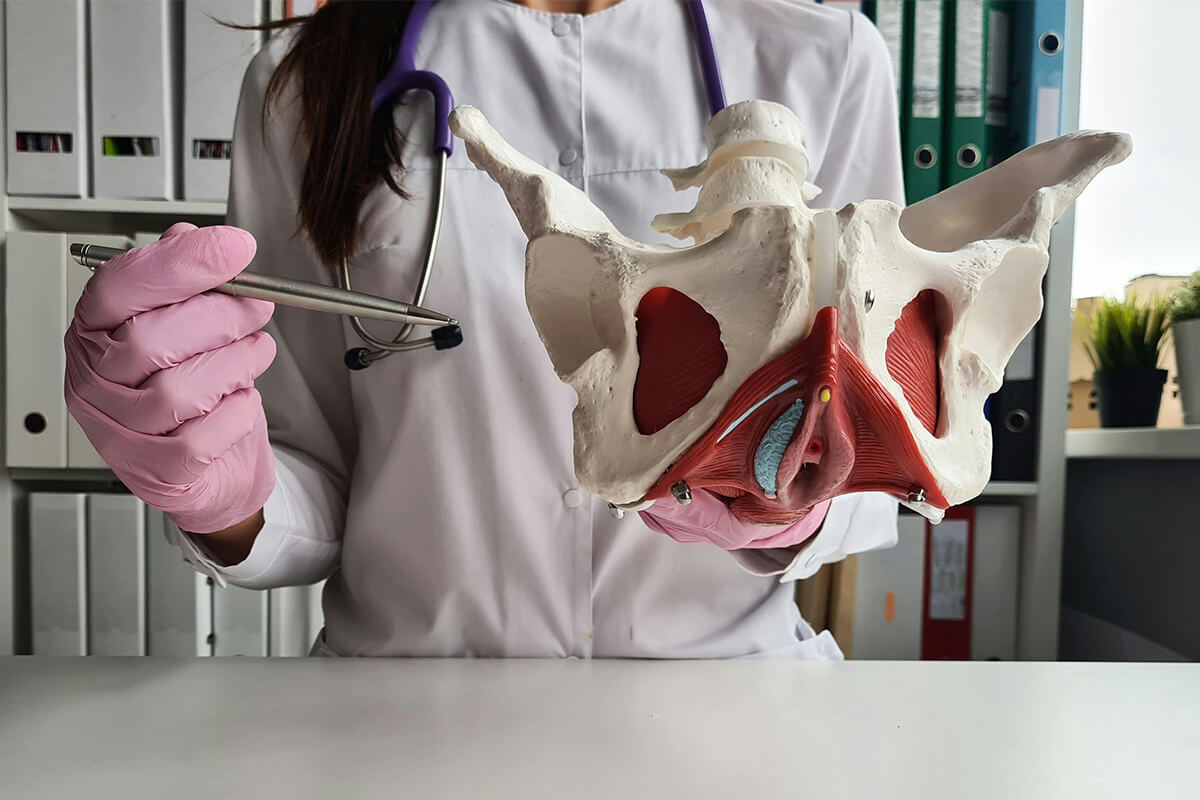
Understanding hypertonic vs. hypotonic pelvic floors: symptoms and treatment protocols
When it comes to pelvic health, understanding the differences between hypertonic and hypotonic pelvic floors is crucial.

How to strengthen your pelvic floor muscles without “Kegels”?
Tired of the same old Kegel routine? Whether traditional pelvic floor exercises leave you feeling uncomfortable or just aren't cutting it anymore, it's time to shake things up.

Is pelvic floor electrical stimulation right for you? Understanding the side effects
Ever wondered about electrical stimulation to help zap your way to a healthier and stronger pelvic floor. Pelvic floor electrical stimulation is gaining buzz, but it's not without potential side ef...
